- Daftar wilayah metropolitan menurut jumlah penduduk
- Hyperparathyroidism
- Secondary hyperparathyroidism
- Tertiary hyperparathyroidism
- Primary hyperparathyroidism
- Parathyroid disease
- Parathyroid gland
- Evocalcet
- Renal osteodystrophy
- Calcium-sensing receptor
- Calcimimetic
- Possibly secondary hyperparathyroidism : r/hyperparathyroidism
- Secondary Hyperparathyroidism? : r/hyperparathyroidism - Reddit
- Secondary vs Tertiary Hyperparathyroidism in CKD : r/step1 - Reddit
- Is this secondary hyperparathyroidism and how to fix it?
- Hyperparathyroidism - Lessons Learned 1/n : r/Parathyroid
- Anyone been treated with vitamin D and not need surgery?
- Very low Vitamin D. Slightly high calcium. : r/Parathyroid ... - Reddit
- Can anyone explain diff between secondary and tertiary ... - Reddit
- Confirmed primary hyperparathyroidism but Dr is refusing to do …
- Has anyone dealt with secondary hyperparathyroidism and what …
secondary hyperparathyroidism
Secondary hyperparathyroidism GudangMovies21 Rebahinxxi LK21
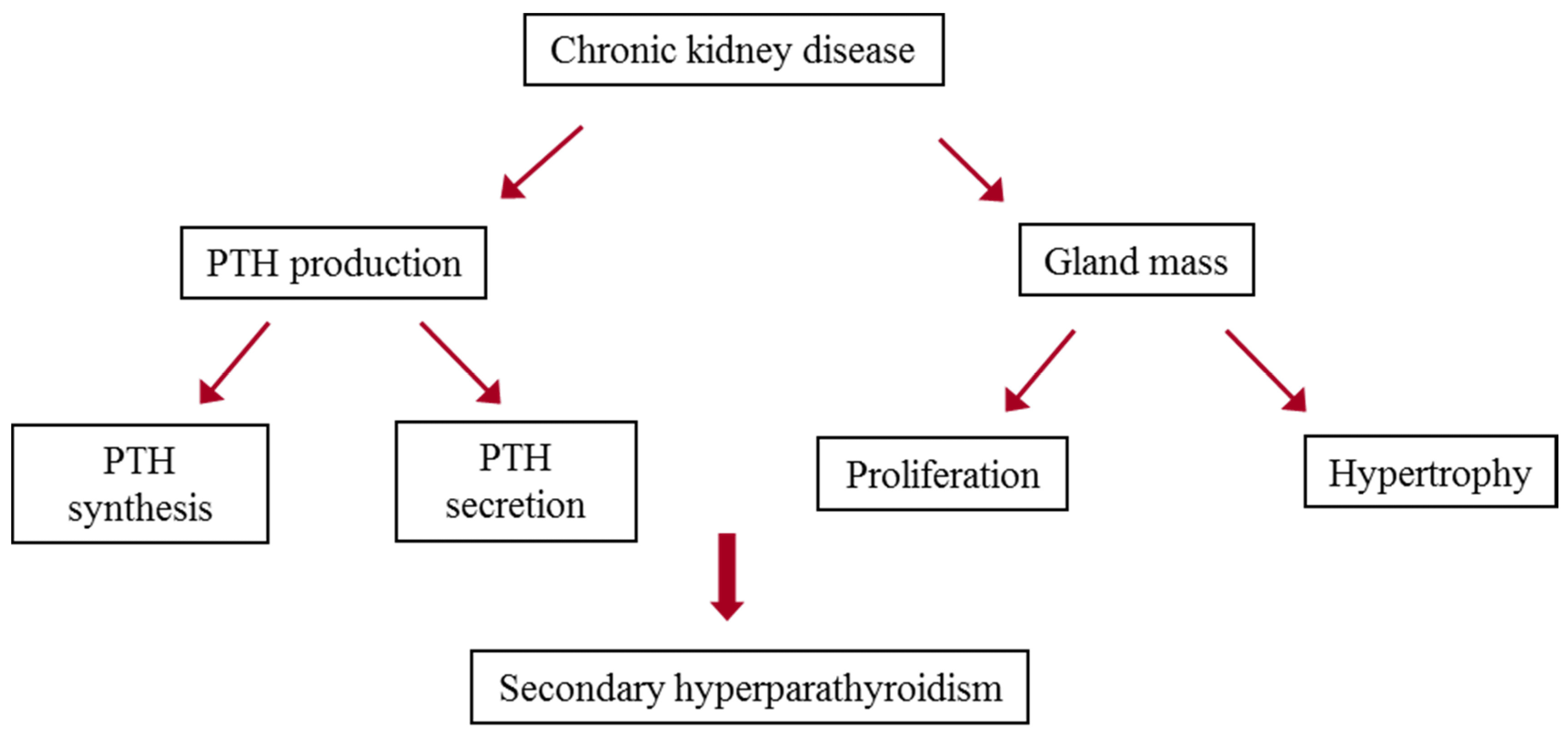
Secondary hyperparathyroidism is the medical condition of excessive secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia (low blood calcium levels), with resultant hyperplasia of these glands. This disorder is primarily seen in patients with chronic kidney failure. It is sometimes abbreviated "SHPT" in medical literature.
Signs and symptoms
Bone and joint pain are common, as are limb deformities. The elevated PTH has also pleiotropic effects on the blood, immune system, and neurological system.
Cause
Chronic kidney failure is the most common cause of secondary hyperparathyroidism. Failing kidneys do not convert enough vitamin D to its active form, and they do not adequately excrete phosphate. When this happens, insoluble calcium phosphate forms in the body and removes calcium from the circulation. Both processes lead to hypocalcemia and hence secondary hyperparathyroidism. Secondary hyperparathyroidism can also result from malabsorption (chronic pancreatitis, small bowel disease, malabsorption-dependent bariatric surgery) in that the fat-soluble vitamin D can not get reabsorbed. This leads to hypocalcemia and a subsequent increase in parathyroid hormone secretion in an attempt to increase the serum calcium levels. A few other causes can stem from inadequate dietary intake of calcium, a vitamin D deficiency, or steatorrhea.
Diagnosis
The PTH is elevated due to decreased levels of calcium or 1,25-dihydroxy-vitamin D3. It is usually seen in cases of chronic kidney disease or defective calcium receptors on the surface of parathyroid glands.
Treatment
If the underlying cause of the hypocalcemia can be addressed, the hyperparathyroidism will resolve. In people with chronic kidney failure, treatment consists of dietary restriction of phosphorus; supplements containing an active form of vitamin D, such as calcitriol, doxercalciferol, paricalcitol; and phosphate binders, which are either calcium-based and non-calcium based.
Extended Release Calcifediol was recently approved by the FDA as a treatment for secondary hyperparathyroidism (SHPT) in adults with stage 3 or 4 chronic kidney disease (CKD) and low vitamin D blood levels (25-hydroxyvitamin D less than 30 ng/mL). It can help treat SHPT by increasing Vitamin D levels and lowering parathyroid hormone or PTH. It is not indicated for people with stage 5 CKD or on dialysis.
In the treatment of secondary hyperparathyroidism due to chronic kidney disease on dialysis calcimimetics do not appear to affect the risk of early death. It does decrease the need for a parathyroidectomy but caused more issues with low blood calcium levels and vomiting.
Most people with hyperparathyroidism secondary to chronic kidney disease will improve after renal transplantation, but many will continue to have a degree of residual hyperparathyroidism (tertiary hyperparathyroidism) post-transplant with associated risk of bone loss.
Prognosis
If left untreated, the disease will progress to tertiary hyperparathyroidism, where correction of the underlying cause will not stop excess PTH secretion, i.e. parathyroid gland hypertrophy becomes irreversible. In contrast with secondary hyperparathyroidism, tertiary hyperparathyroidism is associated with hypercalcemia rather than hypocalcemia.
See also
Primary hyperparathyroidism
Tertiary hyperparathyroidism
References
External links
Kata Kunci Pencarian: secondary hyperparathyroidism
secondary hyperparathyroidism
Daftar Isi
Possibly secondary hyperparathyroidism : r/hyperparathyroidism
Jan 22, 2022 · Many people, myself included, also have/had a vitamin D deficiency with primary hyperparathyroidism. But if it’s primary HPT, bringing up your vitamin D levels aren’t going to anything to fix the HPT. The only thing that resolves primary Hyperparathyroidism is surgery because it is only caused by an adenoma.
Secondary Hyperparathyroidism? : r/hyperparathyroidism - Reddit
Mar 31, 2021 · Secondary Hyperparathyroidism? Recent blood work done and I have a PTH of 508pg/mL, calcium of 8.0mg/dL and vitamin D of 19ng/mL. PTH is extremely high and am kind of concerned about it.
Secondary vs Tertiary Hyperparathyroidism in CKD : r/step1 - Reddit
Apr 20, 2019 · The answer was secondary hyperparathyroidism (decreased Ca, increased PO4, increased PTH), which makes sense. Can someone explain how to distinguish between this and tertiary hyperparathyroidism given only the clinical scenario (in tertiary, PTH and Ca would be elevated)? What would the PO4 levels be in tertiary hyperparathyroidism?
Is this secondary hyperparathyroidism and how to fix it?
May 19, 2024 · It does sound like this could be secondary hyperparathyroidism, and if your surgeon can't help you with treatment, you should seek help with another doctor. The obvious thing right now would be to start supplementing with cholecalciferol (vitamin D3).
Hyperparathyroidism - Lessons Learned 1/n : r/Parathyroid
Sep 18, 2023 · The only treatment for primary hyperparathyroidism is surgical removal of one or more of the four glands. In the hands of an experienced endocrine surgeon this is a procedure with a cure rate of close to 100%.
Anyone been treated with vitamin D and not need surgery?
Jan 23, 2022 · If it’s true secondary hyperparathyroidism, then yes a vitamin D regiment should help restore a balance to the PTH and calcium levels in the body (I’m not a doctor). However, in all I’ve read, no increase in vitamin D will cure PHPT. Only surgery. Medical treatment only really treats the symptoms as far as I’ve been told.
Very low Vitamin D. Slightly high calcium. : r/Parathyroid ... - Reddit
May 1, 2024 · The way the parathyroid feedback loop works (or rather doesn't work) in primary hyperparathyroidism is this: The parathyroid tumor produces excessive PTH with very little regard to what your calcium level is. This causes vitamin D to convert and lowers your vitamin D level.
Can anyone explain diff between secondary and tertiary ... - Reddit
Jun 30, 2021 · Secondary and tertiary hyperparathyroidism both occur in the setting of CKD, however, tertiary occurs much later in the disease process. Over time the PT gland loses its regulatory systems due to chronic stimulation in ckd due to hypocalcemia and hyperphosphatemia.
Confirmed primary hyperparathyroidism but Dr is refusing to do …
Apr 2, 2022 · I have primary hyperparathyroidism confirmed by my endocrinologist and am symptomatic. She ordered a DEXA scan and said I don't qualify for surgery because my bone density is normal. She wants me to keep supplementing with vitamin D and just do annual bloodwork but I feel like there's no way I'm going to feel better unless I have surgery.
Has anyone dealt with secondary hyperparathyroidism and what …
May 19, 2024 · High pth levels since 2020 I'm 35 female and my recent blood results are concerning me. I have an appointment on Thursday with my surgeon (who looks…